What began as a bold experiment—creating life outside the human body—has become a lifeline for millions. Since the birth of the first IVF baby in 1978, science has transformed hope into reality, yet the journey to parenthood remains as emotional and challenging as ever.
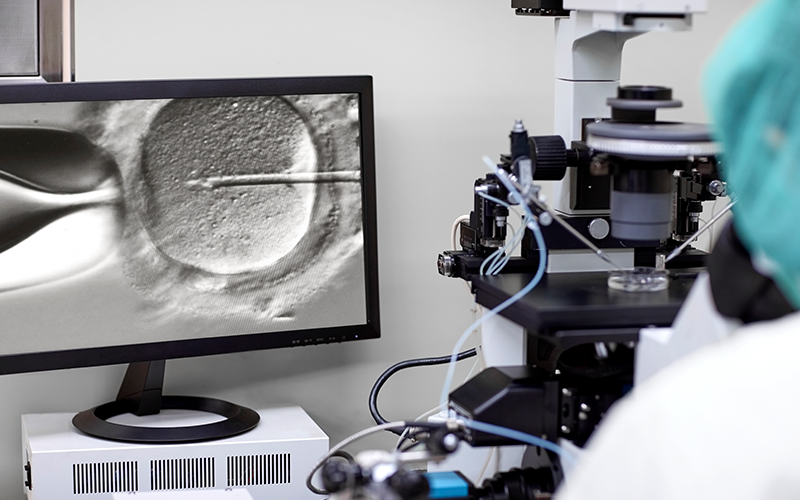
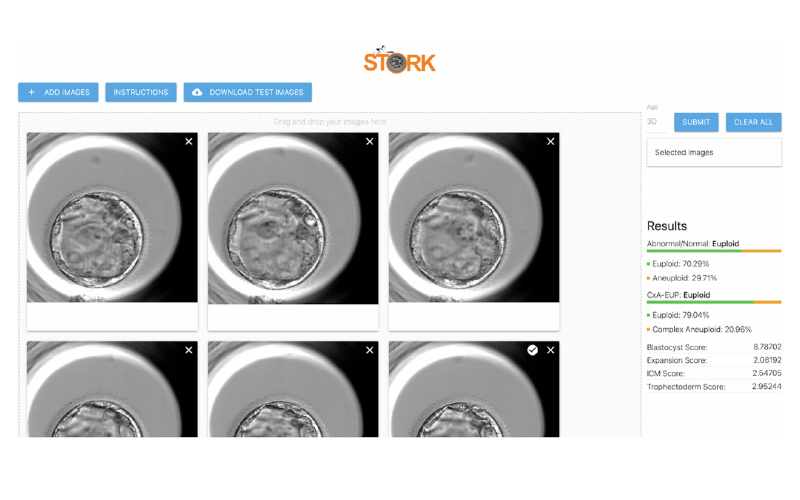
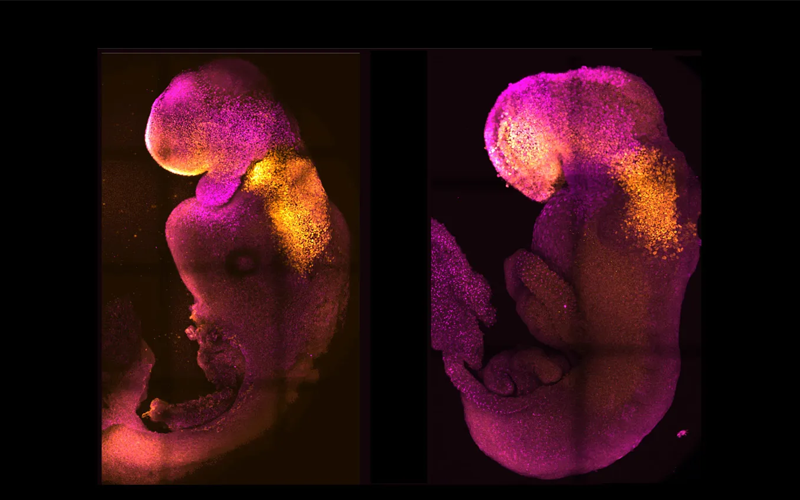
Today, IVF is not just about overcoming infertility. It's about pushing the boundaries of reproduction itself, with AI selecting embryos, stem cells creating gametes, and synthetic life inching closer to possibility.
How far have we come—and how far are we willing to go?