{{ vm.tagsGroup }}
05 Jan 2026
7 Min Read
Dr Foo Jhi Biau (Academic Contributor), Nellie Chan (Editor)
For decades, treatments for inflammatory and degenerative diseases have focused on managing symptoms rather than repairing damage. Long-term steroids and immunosuppressants come with heavy side effects, and curative options are often out of reach. But what if we could shift from simply controlling decline to actively restoring health?
At Taylor’s University, Dr Foo Jhi Biau is exploring exactly that possibility. His research centres on mesenchymal stem cell–derived exosomes—nanosized vesicles released by cells that have the remarkable ability to modulate inflammation and stimulate tissue regeneration. Through the lens of regenerative medicine, he is investigating how these tiny particles could pave the way for targeted, cell-free therapies.
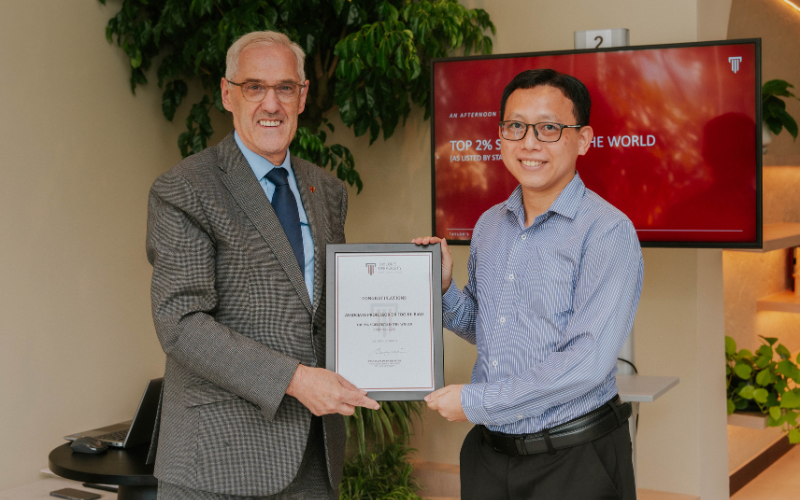
Ranked among the world’s top 2% of scientists for 2025 by Stanford University, Dr Foo is an associate professor at the School of Pharmacy. This recognition reflects his influential contributions to regenerative medicine, where his work is exploring new frontiers in treatment development.
In his current research, he focuses on exosomes rather than live stem cells for medical applications, as the latter carry safety risks, variability, and regulatory complications. This shift in emphasis enables controlled, targeted, and potentially safer therapies, while also creating opportunities for more stable and scalable solutions.
We spoke with him to understand the science behind his work, the challenges of translating a new therapeutic platform, and the long-term impact it could hold for Malaysia and beyond.
Q: For someone unfamiliar, how would you describe your research?
A: My research seeks to develop innovative medical treatments using mesenchymal stem cell (MSC)–derived exosomes. In regenerative medicine, this approach is known as ‘cell-free therapy,’ which harnesses the therapeutic benefits of cell secretions rather than the cells themselves. These nanosized vesicles hold great potential for suppressing inflammation and supporting tissue regeneration.
Q: What inspired you to explore exosomes as a therapeutic platform?
A: Many patients with inflammatory diseases rely on long-term steroids or immunosuppressants, which can take a serious toll on their quality of life. Exosomes offer a safer alternative by providing the regenerative benefits of stem cells while avoiding the associated risks.
Q: What key gap does your research aim to fill?
A: Degenerative diseases currently have no cure—existing treatments mainly manage symptoms. My work aims to develop regenerative solutions that can repair and restore damaged tissues, addressing areas where conventional medicine falls short.
Q: Did you encounter any breakthroughs during your research?
A: Yes! We successfully stabilised exosomes in a dry powdered form that remains effective for at least six months. This overcomes the need for ultra-cold storage, a major barrier in clinical use, and has been patented. The breakthrough could transform large-scale production, storage, and distribution, making these therapies more accessible to patients.
Q: What makes working with MSC-derived exosomes particularly challenging?
A: Working with MSC-derived exosomes presents several unique challenges. MSCs naturally vary from donor to donor, which can affect the consistency and reproducibility of the exosomes they produce. The field of regenerative medicine is highly regulated, and rightly so—ensuring therapies meet safety and quality standards is essential before they can be approved for clinical use. Exosomes themselves are fragile, requiring stabilisation to maintain their therapeutic properties. Finally, the costs of developing and producing these therapies must be carefully managed to ensure they remain accessible and affordable for patients.
Q: What are some common misconceptions about your research?
A: A major misconception is that stem cell products—whether formulations, preparations, or therapies—are unregulated. In reality, the National Pharmaceutical Regulatory Agency (NPRA) has clear guidelines that researchers, clinicians, and investors must adhere to. Another misconception is that all exosomes naturally accumulate at damaged tissues. While they can target injury sites, this does not occur consistently, which is why local delivery methods are preferred for precision.
Q: How do you navigate the regulatory landscape while maintaining scientific innovation?
A: Navigating the regulatory landscape while maintaining scientific innovation is all about striking the right balance. Current regulations distinguish between minimal and extensive manipulation of cells, particularly in the production of exosomes. To stay aligned, we deliberately minimise cell manipulation, helping us meet safety standards and regulatory requirements as we move towards clinical trials and product registration. This approach protects the scientific integrity of our work while increasing the likelihood that our therapies reach patients safely and effectively.
Q: Why is this research particularly relevant right now?
A: Regenerative medicine, especially cell-free therapy, is rapidly establishing itself as the future of healthcare. Our research is timely because it addresses major health challenges, including lung diseases, skin disorders, and neurodegenerative conditions—areas where more effective treatments are urgently needed.
Q: What long-term difference could your research make?
A: Over the long term, the impact of this research could reach far beyond patient care. Successful outcomes may not only deliver new therapeutic options but also attract investment, foster collaborations with leading scientists, and strengthen Malaysia’s presence and competitiveness in the global biotechnology landscape.
Q: What steps are needed to translate the research into therapies for clinical and commercial use in Malaysia?
A: Translating this research into therapies for clinical and commercial use in Malaysia requires several coordinated steps. Strong partnerships between hospitals, universities, and biotech companies are essential to accelerate the journey from research to real-world therapies. We're already collaborating with industry and hospital partners to support translational studies.
Clear commercialisation pathways—supported by government initiatives, innovation hubs, and entrepreneurial funding—can help bring promising ideas to market. While regenerative medicine was initially driven by government investment, increased industry participation is now crucial for the sustainable delivery of therapies to patients.
Scalable production systems are also critical. Establishing GMP (Good Manufacturing Practice)-grade facilities and using standardised, minimally manipulated cell production processes ensures therapies meet safety and regulatory standards. In our work, we use standardised isolation methods that support smoother translation into clinical use.
Q: How has your academic journey shaped your approach to this pioneering field?
A: During my PhD, I trained in compound isolation from plants, learning techniques in separation and purification that I now apply to isolating exosomes. I also developed skills in cell handling, which have been crucial for working with these delicate vesicles. These foundations built my confidence and resilience, equipping me to pursue the rigorous field of exosomes—a then-relatively unexplored area—since 2017.
Q: Can you share a personal insight or defining moment from this project?
A: Venturing into a niche field is never easy, especially when it’s largely uncharted. One defining moment for me was achieving a breakthrough that confirmed we were at the forefront of this research, gaining recognition both nationally and internationally. This experience reinforced the importance of courage, persistence, and collaboration with dedicated researchers in driving meaningful progress.
Q: What advice would you give to young researchers aiming to work in this field?
A: For young researchers interested in regenerative medicine and exosome research, my advice is to first understand Malaysia’s regulatory landscape, including how products are classified and what counts as minimal or extensive manipulation, as even the most promising therapies cannot reach patients without compliance. Building strong connections with industry is also crucial, as partners provide practical insights, sustainable funding, and clear pathways for translating research into clinical or commercial applications. Finally, stay engaged with the global research community—collaborating internationally, exchanging knowledge, and sharing ideas—to strengthen expertise and stay ahead of emerging scientific developments.
Dr Foo’s work is still evolving, but its implications are far-reaching. By demonstrating that MSC-derived exosomes can be stabilised, stored, and optimised for therapeutic use, he is laying the groundwork for treatments that could repair and restore damaged tissues, reduce inflammation, and offer relief to patients with currently incurable diseases.
Next, he is advancing his research by developing targeted delivery systems to guide exosomes to their intended tissues and by building industry partnerships to move discoveries toward clinical trials. These efforts bring his laboratory findings closer to practical application, helping make cell-free therapies accessible to patients in Malaysia and beyond.
By transforming tiny biological messengers into ‘mighty medicine,’ Dr Foo’s work shows that even the smallest particles can hold enormous potential.