(Updated 30 November 2021)
{{ vm.tagsGroup }}
05 Jun 2020
7 Min Read
Ailyn Low (Guest Contributor)
(Updated 30 November 2021)
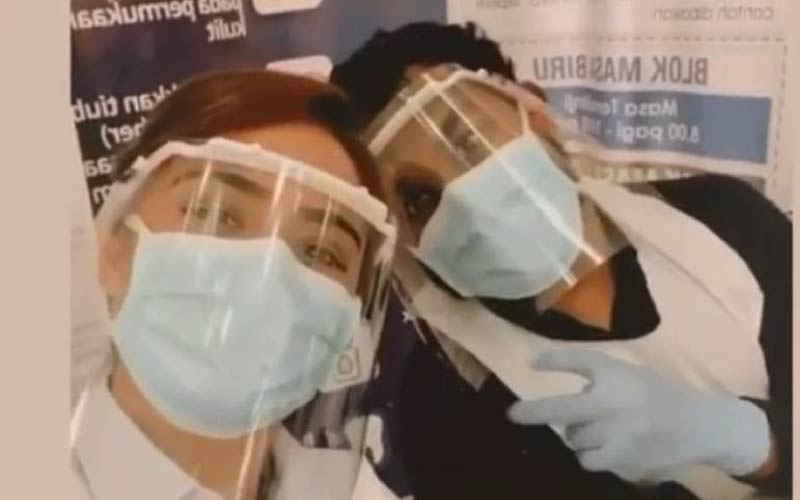
Life as a frontliner is tough, but what exactly do they go through? Dr. Mahes shares his experience. |
Ever since he was 5 years old, Dr. Mahes Arvin Premananth had the noble intention most medical professionals possess — the desire to save the lives of people suffering. That’s what led him to pursue a Bachelor of Medicine and Bachelor of Surgery (MBBS) at Taylor’s University.
But, with the pandemic, how does it feel being exposed to the virus and possibly risking the lives around him? Our 2019 Taylor’s School of Medicine alumni shares his experience as a doctor during the pandemic at Hospital Sungai Buloh.
Q: What inspired you to study medicine?
A: I wanted to be an interventional cardiologist ever since I was 5 years old. My grandfather had a massive Myocardial Infarction (MI) at that time and no options were given to him other than a coronary bypass. I always thought, “Why couldn’t he visit a cardiologist and undergo stenting?”
That gave me the passion to save people suffering from heart disease in the future and improve their quality of life. That’s why I intend to specialise Interventional Cardiology.
Q: What was it like on your first day of work? Have you changed over time?
A: It’s been 5 months since being placed in Hospital Sungai Buloh. Honestly, it was really overwhelming at first. I had to deal with so many mixed feelings and being scared and panicky was definitely a part of it. I constantly felt like becoming a student all over again.
Now, I definitely feel a whole lot braver, confident, and bolder in approaching my patients and coming up with a management plan for them. Looking back, I think it’s amazing to see that kind of improvement in myself.
Q: How did your working hours and experience change with MCO and COVID-19?
A: Working hours definitely changed with the presence of COVID-19. I used to be working 67 hours a week with only a day off. Now, it has dropped to 50 hours a week with 2 days off so as to reduce our exposure to the disease itself.
When MCO was strictly implemented, working hours were still 50 hours a week which made us feel safer because we knew our exposure to the cases were lesser. However, there was still work stress and the mental implication was there. Every day, I would be going home worried with the thought of what would happen if I brought the virus home. Would I infect my whole family and all my loved ones? Their safety was definitely my concern too.
Q: What measures have you taken when going back home?
A: So, throughout these few months, I’ve actually been practising self-quarantine in a different room from everyone else with minimal face-to-face contact. That’s how the pandemic has affected us as doctors and the way we interact with our loved ones.
Q: How does it feel treating COVID-19 patients? What are the best and worst moments for your COVID-19 cases?
A: The worst moment is like what I said earlier. It’s not knowing if I’ve carried the bug home and possibly spreading it to my loved ones. I feel like I’m constantly living life on the edge. Kind of like Tom Cruise! But even with that, it feels amazing to be serving as a frontliner during the pandemic.
The best moment for me would definitely be seeing a critically ill patient, who’s been intubated and was actually on the verge of dying, taking a 180° turn and suddenly appears all healthy with good fighting strength. Eventually, these patients will be discharged because they’re fully cured.
Q: How has your education prepared you with handling the current situation?
A: I would say that I’ve been relatively well-exposed and received good theoretical knowledge of different diseases. For me, studying at Taylor’s, with the affiliation with Hospital Sungai Buloh, gave me exposure to cases like HIV, Hantavirus, Malaria, Tuberculosis, etc. So, it did prepare me to see a new strand of disease not known to mankind. I roughly knew the protocols, steps, and precautions that are needed to be taken when dealing with such airborne diseases.
Also, it made my working life a whole lot easier. I remember my consultants asking me, “Hey, do you know the donning and doffing of the Personal Protective Equipment (PPE)?” And I was so happy because I knew the basic protective equipment protocols which I learnt throughout my years with Taylor’s as well as during my clinical elective programmes abroad. This really made me feel much safer.
Q: Any words for aspiring doctors?
A: Always have a goal from the start of your student life and aim higher than it. Nothing is impossible. They used to say that it’d be impossible for a Malaysian or anyone, for that matter, to go to the moon. But look at us now! We’re growing in ways we’ve never thought possible so be proud of every step you take. Whether it’s a failure or a success because failure’s just another word for growth.
Q: If you could tell the community something, what would it be?
A: I know it’s not easy living in this so-called ‘new normal’. But that’s what we have to do as a team, as a nation, to help eradicate this disease from our planet. Even if it’s just little baby steps that we need to practise.
Many people see articles which say wearing masks doesn’t help but how reliable are those articles? Do we really know?
All the simple things we can do like wearing masks, using hand sanitiser, and practising social distancing do play a role in a long-term strategy to help reduce our nation to a zero-COVID nation.
It might be uncomfortable or suffocating wearing those masks but hey, if we don’t help ourselves, who will? It’s important to remember that we, doctors, aren’t the only frontliners. You play a role too! Take care and stay safe everyone!
After one year since the first interview, we checked in to find out how Dr. Mahes has settled in as a frontliner.
Q: Over the past 1 and a half years, has your work life during the pandemic changed much? Is there anything you wish would happen?
A: Work has definitely been more hectic especially when cases were surging into 20k daily. Our workload in the hospital kept overflowing, beds were fully occupied, and ICUs full. Honestly, it wasn’t easy. It STILL isn’t easy. My only wish is for the cases to dip to a single digit but, realistically, it’ll be a long-term process.
Q: Were there any significant and memorable events over the past year in your career as a doctor?
A: As a doctor of course there are tons of moments and events in our career that we keep close to our hearts. Losing a patient, going all out to save a patient, etc. The list is never ending.
Q: You mentioned your intention of specialising in Interventional Cardiology. How is the progress towards that?
A: Being a contract doctor in Malaysia at this point of time means we don’t get a chance to enter the local government Master’s programme offered. Hence, I've to work on my own parallel pathway, forking out my own money and expenses to head towards that journey. I’d say I’m making baby steps in the aim of reaching that position one day.
Q: At the start of your career, you felt scared and panicky but since then, you’ve built yourself to be braver, confident, and bolder. How do you feel about your progress now?
A: Definitely! I feel much happier, bolder, and braver now as compared to when I first started. I still remember my first night of duty where I was left alone to man an acute ward of 30 patients. I felt chills down my spine all the time. A long way has come since then, and now, when I’m making crucial decisions, it comes more naturally and the fearful or panicky feeling is the least of my concerns.
Q: With us now being in the endemic stage, what is life like for you as a doctor that not many are aware of? Is there any advice you can give others out there?
A: Despite us being in the endemic stage and vaccination rates going up, people still need to be aware that COVID-19 is still around. You may not be admitted under Category 5 cause nobody develops that stage immediately but it’s a process. People believe that once you’re vaccinated, you can breach SOPs and not worry about anything but the reality is that your chances of getting the virus is still relatively high — what more with the new variant. The point of vaccination is to reduce the severity of symptoms, not being completely protected from it. Trust me, I’ve been vaccinated since March 2021 yet contracted it myself 2 months later!
Q: What are your thoughts on the Omicron variant and how can we prepare ourselves if it comes to Malaysia?
A: Well, I’m sure you’ve heard that the USA reported their first case recently and Malaysia detected its first case of Omicron too, 3rd December 2021! It’s unclear yet whether the Omicron strain is more susceptible than the Delta strain because research is still ongoing. That being said, we need to prepare for the worst and be on guard. Most countries are preparing for their 4th wave and Malaysians need to start being on the lookout for that.
I still see malls being full and, what’s worse, is seeing babies and toddlers out and about. We need to realise that the battle isn’t over. Cases are still rising, our hospital beds are filling up. I’m currently working at Sungai Buloh ICU and I can tell you that our beds are at maximum capacity already. Please, we’ve to stay alert, especially now.
Find out how you can build a foundation in medicine here. |